Headaches and Migraine
Cervicogenic Headache
A cervicogenic migraine is a type of headache that originates from issues in the cervical spine or neck region. Unlike typical migraines that arise from abnormalities in the brain, cervicogenic migraines are associated with structural problems in the neck, such as misalignment of the cervical vertebrae, muscle tension, or nerve compression.
The pain in cervicogenic migraines is usually one-sided and can be intense, throbbing, or pulsating. Individuals may experience symptoms such as neck pain, stiffness, and limited range of motion in the neck. The headache often begins in the neck and then radiates upward, causing pain on one side of the head. It can also be accompanied by visual disturbances, nausea, and sensitivity to light and sound, similar to other types of migraines.
Cervicogenic migraines are often triggered or exacerbated by poor posture, neck trauma, prolonged periods of sitting, or repetitive neck movements. Diagnosis of this condition involves a thorough examination by a healthcare professional, and it may include imaging studies to identify any structural abnormalities in the cervical spine.
Trigger Point Therapy for Headaches
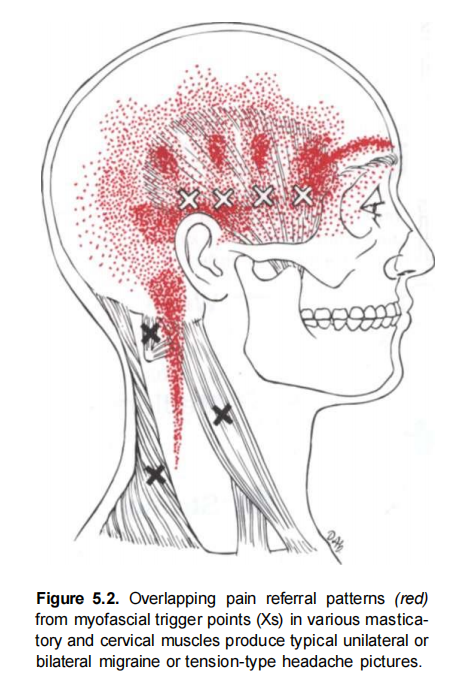
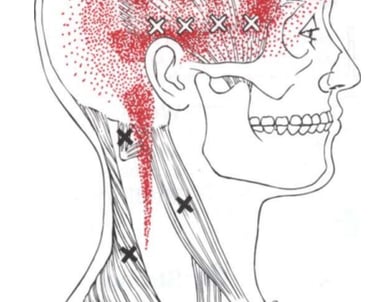
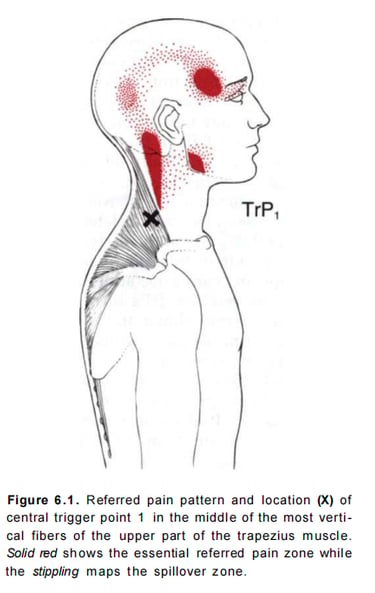
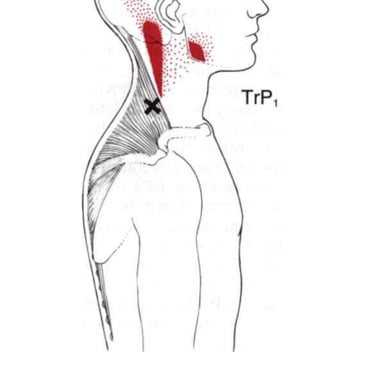
Trigger point therapy is a form of manual therapy that involves applying pressure to specific points on the body known as trigger points to alleviate pain and discomfort. When it comes to headaches, trigger point therapy is often used to address tension-type headaches and migraines by targeting trigger points in the neck, shoulders, and head.
Here's an overview of how trigger point therapy may be applied for headaches:
Identification of Trigger Points:
A trained healthcare professional, such as a massage therapist, physical therapist, or chiropractor, will identify trigger points associated with headache pain. These trigger points are areas of muscle tightness or knots that may refer pain to other parts of the body, including the head.
Application of Pressure:
The therapist will apply direct pressure to the identified trigger points using their fingers, thumbs, or specialized tools. The pressure may vary based on the individual's tolerance and the severity of muscle tension.
Release of Tension:
The sustained pressure on the trigger points aims to release muscle tension and improve blood flow to the affected area. This can help reduce pain and discomfort associated with headaches.
Stretching and Manipulation:
In addition to applying pressure, therapists may incorporate stretching and manipulation techniques to further relax and release tension in the muscles. This can enhance the overall effectiveness of trigger point therapy.
Home Exercises:
Therapists often provide patients with specific exercises or stretches to perform at home to complement the in-office trigger point therapy sessions. These exercises may help prevent the recurrence of trigger points and promote long-term relief.
Hydration and Lifestyle Recommendations:
Therapists may also offer advice on lifestyle factors that can contribute to muscle tension and headaches. Adequate hydration, proper ergonomics, and stress management strategies are examples of recommendations that may be provided.
It's important to note that while trigger point therapy can be beneficial for some individuals with headaches, it may not be suitable for everyone. It's essential to consult with a healthcare professional to determine the underlying cause of headaches and to develop a comprehensive treatment plan that may include trigger point therapy along with other appropriate interventions.
ADDRESS
10255 Commerce Dr. Suite 148
Carmel, IN 46032
